COVID-19 cases and deaths at U.S. nursing homes are once again on the rise.
According to Centers for Disease Control and Prevention data, Illinois saw its highest-ever case rate for nursing home residents this month, recording 2,284 cases for the week ending Jan. 9. That surpassed the previous weekly record of 2,131 cases set in December 2020.
Cases among staff have also reached record levels. And while resident deaths are on the rise too, the numbers are still far short of previous records – even though experts caution that deaths are a lagging indicator.
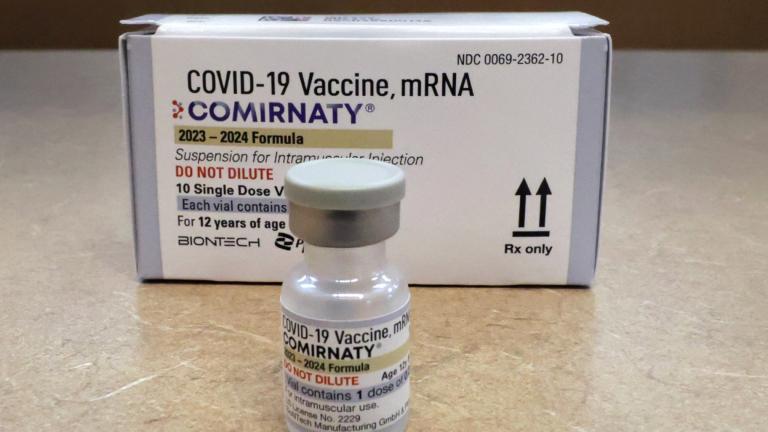
Tamara Konetzka, a University of Chicago professor who specializes in public health and geriatrics, said when vaccines first became available to nursing home residents and staff about a year ago it drastically reduced cases and deaths. But because of resident and staff turnover, among other factors, that vaccination campaign alone wasn’t enough.
“We also know that these are older adults who sometimes have weaker immune systems than the rest of the population, they may not have as much of a reaction to begin with to the vaccines, and their immunity may wane more quickly over time,” Konetzka said.
Konetzka says continuing to promote vaccines and boosters, as well as ensuring access to testing and PPE, are critical to keeping case rates down.
Joseph Quayson, director of nursing at Alden Park Strathmoor in Rockford, says while his facility is currently fully staffed, it’s taken pulling in managers and other outside help to continue meeting residents’ needs during the surge.
“Staffing has been a major problem for us. With the increase in cases of COVID, a lot of staff members have to be off work, and that is putting a constraint on the rest of the staff left behind to pick up the slack,” Quayson said.
Another factor that may affect nursing homes: the upcoming federal mandate for health care workers at facilities that accept Medicare and Medicaid. Staffers have until the end of February to get vaccinated or obtain a medical or religious exemption. Konetzka says that’s a stricter requirement than the state’s vaccination rules for health care workers, which allow unvaccinated staff to get regularly tested instead.
“The hope would be that vaccination rates among nursing home staff will go up because they won’t any longer have that testing option,” Konetzka said. But Konetzka notes there’s another wrinkle – the federal mandate won’t apply to the many assisted living facilities that don’t take Medicare or Medicaid, but Illinois’ vaccination-or-test rule does.
“Unless the state decides to change their requirements for assisted living, we will have an odd mix of vaccination requirements being more stringent in nursing homes than in assisted living,” Konetzka said. “I think the industry worries then that staff members who don’t want to be vaccinated will quit their jobs in nursing homes and go down the street to the assisted living facility. It could also have implications for the residents of those facilities, where perhaps we won’t be protecting assisted living residents to the same extent that we do nursing home residents.”
Quayson, who says he supports vaccinations as the best way to prevent COVID-19 cases, deaths and future variants, hopes to see continued education campaigns to reach those who are hesitant. And he’s concerned about more staffing shortages down the road.
“We are paying three times the base rate to get staff to come in and help take care of the residents. With the continuous shortage, there’s competition not only with assisted living but the hospitals right now, because the hospitals need staff and are paying above the base rate to get these staff members to the hospitals,” Quayson said.