Dr. Marina Del Rios was the first person in Chicago to be vaccinated against COVID-19. On Tuesday, the emergency room doctor at University of Illinois Hospital got her second dose of the Pfizer vaccine.
Del Rios, an emergency room physician with nearly 15 years of experience, discusses her experience working amid the pandemic and getting vaccinated.
Below, an edited interview with Del Rios.
What’s it been like being a doctor amid the pandemic?
Del Rios: “It’s been stressful in a way that I don’t recall ever being stressed before. I’m an emergency room doctor right, so you have nights when multiple traumas come in. I remember vividly working in a community hospital on the northwest side of Chicago that served a predominantly immigrant population. I remember vividly one shift where I had five codes come in on one night … that means five people who needed active resuscitation in the emergency department that were close to dying. I remember that night vividly because it was so unusual. That was just a rare, bad night that you would have in months, maybe even years. But now it seems that you are at that brink more than once a week.”
“I’ve had occasions when I’ve basically been running from room to room because I had unstable patients with oxygen levels dropping and requiring intubation and multiple specialty services. … So, it’s just more draining. And also, in the past I wasn’t also so fearful for my own safety. You take care of the trauma and in the case of a heart attack you try to stabilize them, etc. but you are not worried about your own safety and that you might get sick with what this person has.”
“The other part of that is that medicine has become very impersonal in this process. I don’t have the same capacity to connect with patients that I did a year ago. I can’t see them smile or them see me smile.”
How are you and your colleagues coping?
“I know a lot more of my colleagues are seeking help through going to therapy sessions. I myself have sought out a couple. Early on in the pandemic, I had lost a friend and I was also working through figuring out the impact on my own children who had to go from this normal, everyday, taking the bus to school and coming back with their friends to all of a sudden now they are isolated. It was a little bit difficult for me to deal with that. But after a few sessions I found ways of finding joy in things that I do every day. I go running, I put puzzles together.
“I’ve also found that it’s important that you still have your social connections even if you can’t physically see people to make sure that you are checking in with your friends and your family.”
You are among the first Chicago health care workers to have now received two doses of the vaccine. Have you experienced any side-effects?
“The first round all I had was a little bit of soreness around the arm the day after I was immunized. I had my second shot and I am feeling the same thing but I’ve been warned by colleagues of mine who have already gotten, their second dose in other states that you can get quite sick with the second one, meaning more flu-like symptoms, body aches and fevers. So far, I have not experienced that but I’m only on day two.”
How did you feel about getting the vaccine? I’ve read stories saying some healthcare workers and first responders are refusing the vaccine. Did you have any reservations?
“I did not. I’ve obsessively been looking at the data and the research that came out for both the Pfizer and the Moderna vaccines. I’ve asked a lot of questions of people who are more informed than I am regarding the vaccine safety and efficacy. And I felt reassured that this was safe and efficacious and that I should go ahead and get vaccinated.”
“I always think any time that you decide on a procedure or a medication you have to weigh the risk versus the benefits. And for me the risk of getting COVID is so much higher in terms of not only the possibility of me getting COVID, but also if I get COVID I could get very sick and I could die, versus with the vaccine, where the worst that could happen in my mind is that we find out the vaccine is not as effective as it claims to be. But it’s not going to kill me. I may have some discomfort the day after, but it’s not going to kill me. COVID might kill me and so I will take my chances with the vaccine.”
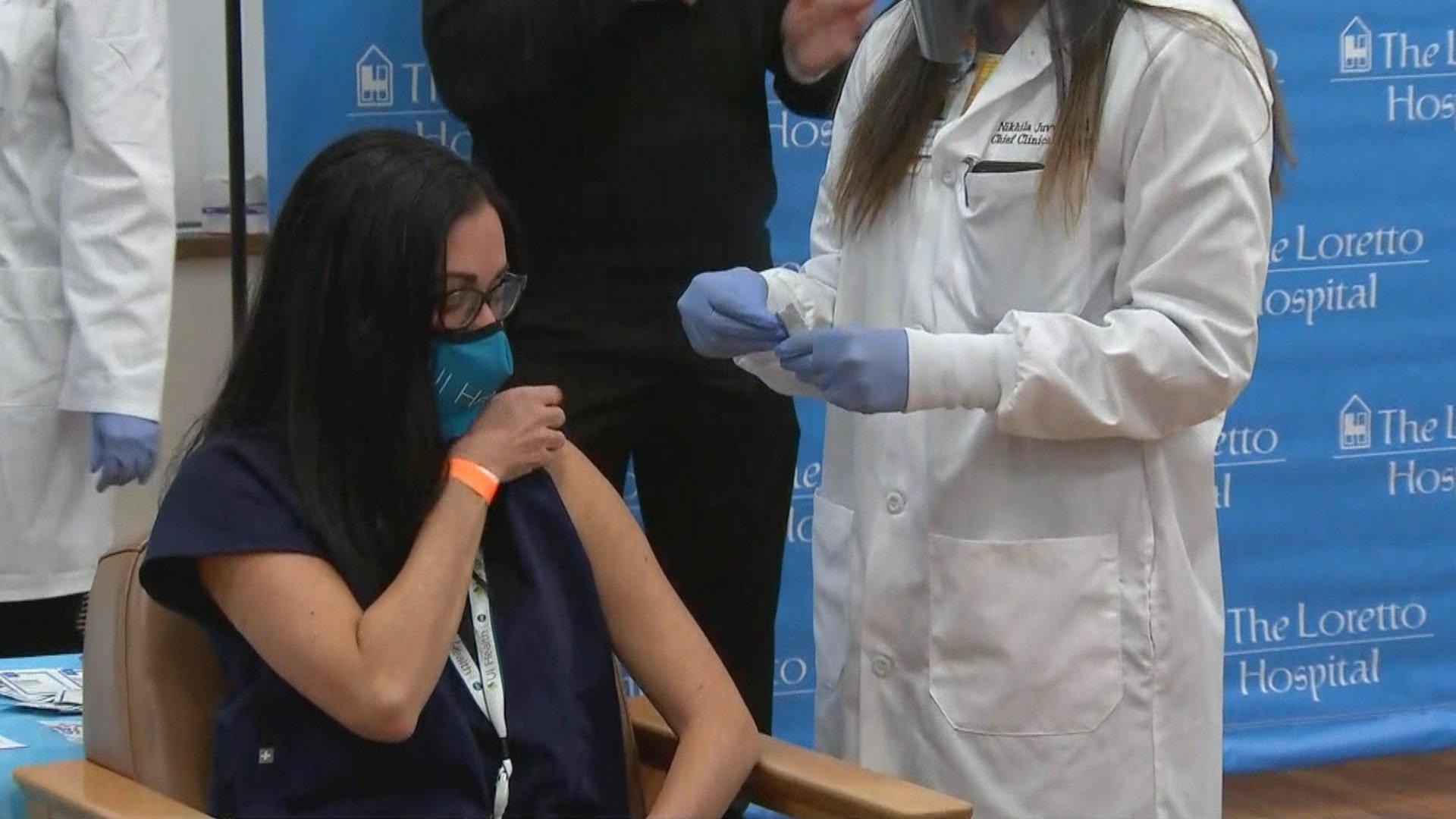 Dr. Marina Del Rios receives the first dose of the COVID-19 vaccine by city officials on Tuesday, Dec. 15, 2020 at The Loretto Hospital. (WTTW News)
Dr. Marina Del Rios receives the first dose of the COVID-19 vaccine by city officials on Tuesday, Dec. 15, 2020 at The Loretto Hospital. (WTTW News)
What about your colleagues? Are they all getting vaccinated or so some have reservations?
“It’s been a very mixed bag. Definitely, all of the emergency physicians that I know in my hospital have either gotten vaccinated or have an appointment to get vaccinated already. With the nursing staff and the EMTs, it’s been a little bit more of a mixed bag, but I haven’t heard ‘I’m not getting the vaccine at all.’ It’s been more of ‘I’m going to wait to see how you guys do.’ They are sort of taking this watchful approach which, although I don’t agree with because I actually think the science is sound, I can understand too that especially in communities where there’s been a history of mismanagement and unethical research and even unethical medical treatment, I can understand why people might want to pause and get more data.”
What would you say to those people who may have concerns about taking a vaccine that has been developed so quickly?
“I think first and foremost is always validating their concerns and then sharing what I know. I think that what you get from the internet and the media is very limited. I find that just sitting down with people and asking them to tell me what their concerns are... and if it’s just about efficacy let me show you the data. And if it’s about safety, well again, let me show you the data.”
“Sometimes people just need to see someone that they know, that they trust, who has gone through it. That’s why I felt it was very important for me to step up, not only as a medical provider but also as a medical provider who is Latina to show my community to say that ‘Hey, I understand your concerns.’ I have voiced those concerns before but I trust the science and I trust it so much that I am willing to set my words into action.”
We’ve seen surging cases across the country since Thanksgiving. What is the situation now at UI Hospital?
“We saw a surge after Thanksgiving and then it never really went back down to the numbers that we had in June, for example, but it did seem to plateau a little bit and we weren’t seeing a constant increase. But we are all worried that we are going to start seeing the Christmas and New Year’s surge now. There’s always a two-to three-week delay in seeing the sicker people.”
What proportion of patients in the emergency department have coronavirus-related issues?
“I would say roughly about a third. At its peak, there was a saying that a colleague of mine would say often on our night shift that ‘everything is COVID,’ because it literally did seem that every patient that we saw regardless of the complaint had COVID. I’m sure it really wasn’t 100%, it was probably closer to 60 or 70%.”
“I’d say now we are at about a third. Most cases are people that may have some flu-like symptoms. We’ll do some bloodwork and. an X-ray and make sure they are not too sick, but generally a lot of those we are able to stabilize and send home with good follow-up and giving them information about warning signs that would have to bring them back to the hospital. But at its peak the hospital was full.”
The lack of enough protective equipment was a big issue in the early part of the pandemic. Do front-line workers now have all the protective equipment they need?
“Now we do. Back in April we got to the point where our supply of PPE was dangerously low. And for me, I have a smaller frame, so the N95 mask that I use is a special smaller size and we had run out of that one entirely. So, what we were being asked to do was return our masks at the end of the shift and they were getting disinfected and then they would return them to us. …
“I’m lucky at my hospital that there’s been enough preparedness and thinking through to make sure that we are not in the same situation that we were in April when our PPE supplies were dangerously low. They are thinking ahead to make sure that we are preparing in case we see the surge that we fear will happen in the next couple of weeks. I know that smaller hospitals in Chicago don’t have the same supplies. And it’s not necessarily because they haven’t thought about it -- it’s just that that they don’t have the money.”