If there’s one thing we’ve learned for certain since the arrival of COVID-19 in the U.S., it’s that nothing is certain, from how the virus is transmitted to how — or even if — we can become immune. No one is dealing with that uncertainty more than the health care workers on the front lines of the crisis.
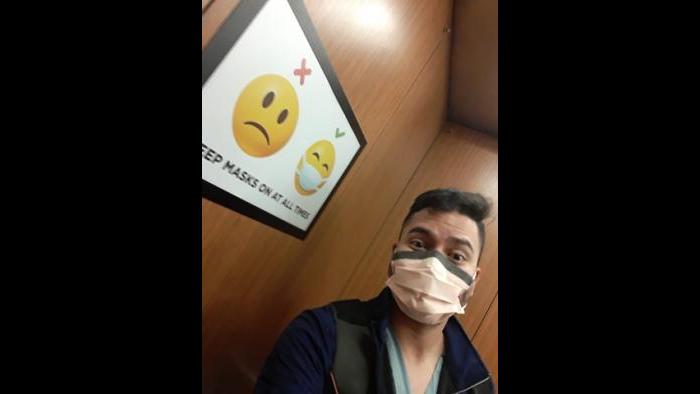
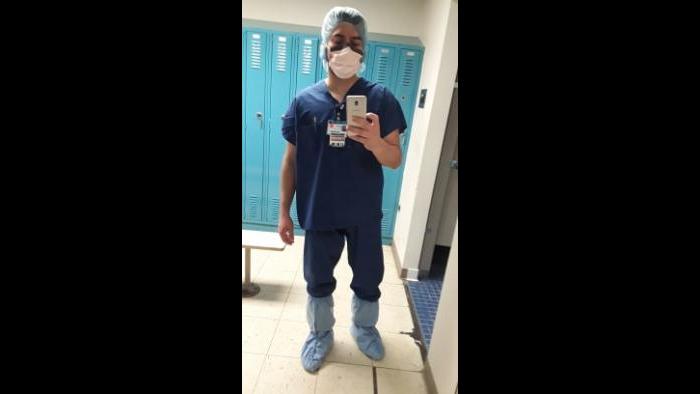
Daniel Ortiz, a registered nurse at UIC Medical Center, has likened his experience of preparing a hospital unit to treat a flood of coronavirus patients to “flying an airplane while building it in the sky.”
He says he was on the job for three weeks after the first COVID-19 patients began to arrive at UIC Medical Center in early March. In late March, Ortiz learned he was one of the nurses assigned to the newly created COVID-19 care unit at the hospital, which necessitated some difficult conversations with his new wife Aimee and their families.
“I told my wife, we’ve got two choices here: I could quit and we could quarantine, or I could go to the hospital and do my thing. People are going to need me more than ever, I’m good at this, but I’m going to get sick. And you’re going to get sick too … But she said, ‘They need someone like you there. Why would I waste you as a human hiding you here with me?’”
Just a couple of days after making the decision to return to work, Ortiz says he felt the onset of COVID-19 symptoms. “I had chills, I had fever, I had a cough, and when I woke up … I had a pounding headache,” he said.
He called in sick and went in for a test the following Saturday.
That was positive test #1.
Ortiz says the symptoms were enough to make him stay home in bed, but they were short-lived.
“I was only in bed sick like that for a day and a half. I called in sick Friday. I woke up Saturday morning and I felt OK,” he said.
At the time, he says, CDC guidelines allowed for him to return to work after six days. Two weeks later, he began to feel sick again. Though the period of illness was again mild and short, he tested positive a second time and was once again sidelined from work.
He tested negative on April 21 and was hoping for a second negative test so he could return to work – but on April 23, he received his third positive result.
On Wednesday, he tested positive once more.
Asked whether he believes he was reinfected, Ortiz says: “I think I was never negative. Because we don’t have that information to say I was reinfected – it was probably a false negative but I can’t say that with certainty.”
While Ortiz acknowledges that this pandemic is unprecedented, he believes that UIC Medical Center should have provided more personal protective equipment for nurses early in the pandemic – a concern he says continues even now.
“I think we have enough ventilators but I don’t think we have enough protective equipment for the nurses,” he said. “I feel like the nurses are handcuffed. They’re asking us to do a job that’s already impossible, but handcuffing our hands behind our back.
“The way nurses work, we adapt really quick – so now we have even more patients assigned to us but we’re more comfortable because we’re getting more of what we need. If you give us the protective equipment we need instead of not giving us the right equipment because there’s a shortage — we were set up to fail. But even then, nurses were still there … We’re bringing people from the brink of death and no one will ever know.”
In a statement responding to those comments, Michael Zenn, CEO of University of Illinois Hospital and Clinics, wrote in part:
“We follow the latest scientific guidelines from local and national public health officials, which have changed dramatically and rapidly over the last few months. All care providers at UI Health haven been provided guidance to use personal protective equipment as recommended by the CDC and in some cases we have implemented recommendations that go beyond the CDC guidelines: in March we were one of the first hospitals in Chicago to implement universal masking of all patients and staff and we have also made non-fit tested N95 and KN95 masks available to staff. Additionally, we implemented testing of all patients on admission and preoperatively on April 16. This greatly enhances our ability to identify and safely isolate patients with COVID-19.”
In the meantime, Ortiz is at home recovering, along with his wife, who has also been ill with what they assume was also a COVID-19 infection. Ortiz says that despite trying to keep their distance, the one-bedroom apartment they share made avoiding transmission almost impossible.
“I would sleep on the couch, drop my clothes at the door and walk straight into the shower. I said, ‘I’ll say hi to you in the morning, and try to keep a distance.’ But it’s a small apartment, there’s no way. We did try. If we would have had a two-bedroom, maybe we would have been able to,” he said.
And despite his firsthand experience with the virus, Ortiz is anxious to get back to work.
“That is where I thrive,” he said. “I know patients need what I can do. I can’t wait to be there.”